Frozen Shoulder: “Unthawing” this Disorder
Most people have heard of this mysterious disorder of the shoulder joint but do not understand what it is. The therapists at OPTSP are very familiar with patients who are dealing with this condition and the joint stiffness, lightning bolt like pain that can accompany it as well as the significant limited mobility and painful interrupted sleep patterns that can occur. What is a frozen shoulder? In the medical world, it is known as “Adhesive Capsulitis”. The incidence rate of this condition is 2% of the general population with 70% of all cases affecting the female gender. It occurs most often in the 40-70 year old age group. The exact underlying cause of this condition remains an enigma although multiple risk factors have been identified. Persons who have had prolonged immobilization of an upper extremity or minor trauma such as impingement syndrome of the shoulder appear more prone to develop this disorder. Other conditions linked to an increased risk include autoimmune diseases, thyroid dysfunction, stroke, Parkinson’s disease, myocardial infarction or post heart surgery, cervical disc disease and diabetic patients. Type I diabetics are at a 5 times greater risk than the general public and Type I diabetics also have a 40% lifetime risk of developing it. It is very rare that a person with a resolved frozen shoulder would ever develop it again in the same arm but up to 30% can develop it in the opposite arm usually within 5 years of original occurrence.
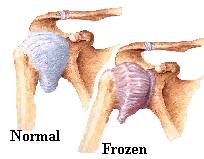
There are two main types of adhesive capsulitis. The first is the “out of the blue” type where onset occurs without prior known incident or trauma causing pain and stiffness. The secondary type occurs when some type of preliminary shoulder issue can be identified that then became complicated and turned into this condition. It is interesting to note that no other joint in the body undergoes a process similar to this disorder. The shoulder joint complex is the most mobile area in our bodies and consists of multiple articulations between the bones of the area (humerus, scapula and clavicle) and all the various muscles, tendons and ligaments that interact to produce and control movement. The other soft tissue that is part of this complex is the fibrous, thick joint capsule that works to support the shoulder joint and even blends with some ligaments and rotator cuff muscles in the area.
Normally, this capsular tissue has relaxed folds in it which allows for freedom of movement. This capsule is also normally lined with a synovial membrane and synovial fluid which contributes to lubricate the joint and allows for smooth capsular movement. With the onset of adhesive capsulitis, there is significant reduction of this lubricating fluid as the joint capsule tissue contracts and adhesions form in the once relaxed folds of this tissue. All of these changes begin to painfully restrict overhead movements and movements that allow for activities of daily living such as brushing/washing hair, dressing, reaching into back pockets or behind your back. Pain occurs and it is difficult to sleep on the involved side.
This debilitating condition is often classified as “self limiting” meaning that there can be a natural resolution of symptoms over time including limited motion gains; however, this spontaneous recovery period can take up to 2 years without medical intervention and very few persons wish to wait this amount of time to improve. Proper medical and orthopedic work up is needed to formally diagnose and to rule out other conditions. Orthopedic management may include joint manipulation under anesthesia, capsule distention techniques with use of saline injections and corticosteroids or actual surgical capsular release with follow up physical therapy. Most often, a conservative approach is tried first with physical therapy being at the front line. The use of proper joint mobilization techniques by a trained therapist can be particularly effective as well as strategic and selective stretching techniques, muscle strengthening and a commitment by the patient to an individually designed home exercise program. Physical Therapy modalities (such as ultrasound, electric stimulation, light therapy, heat and ice), although not effective to eradicate the condition, can be helpful to reduce pain, relax muscles and prepare tissues for mobilization and stretching and to treat tissues after a rigorous therapy session.
Adhesive Capsulitis can be a very painful and debilitating condition. Sleeping ability as well as work place function and activities of daily living are all affected. Physical Therapy remains a cornerstone of treatment for this condition. Treatment is most effective in the hands of experienced and knowledgeable therapists. All of our therapists have extensive expertise in helping with this condition and are well known for our excellent care with multiple shoulder conditions, post surgical shoulder repairs and many upper extremity issues.



